Primary health care data is key to attaining universal health coverage
Strengthening primary health care is key to achieving UHC
The idea that primary health care is the foundation of strong, equitable health systems is not new. In October, health funders, policymakers and practitioners came together in Astana, Kazakhstan to celebrate the 40th anniversary of the 1978 Alma-Ata Declaration and reaffirm their commitment to primary health care as the most equitable and sustainable strategy to achieve health for all.
Yet all too often, primary health care is the weakest link in a health system. Many countries have identified primary health care as an urgent priority, but don’t have the information they need to drive targeted improvements. Uncoordinated data systems that fail to combine local and national-level inputs make it hard to see where primary health care is falling short, and the data that does exist is often of poor quality or difficult for governments and donors to understand and use. With half of the world’s people lacking access to essential health services, most of which can be delivered through strong primary health care, we have an opportunity and responsibility to act now.
The Primary Health Care Performance Initiative (improvingPHC.org) — a global effort to ensure that data on primary health care is both accessible and used to drive decisions with the ultimate goal of transforming the global state of primary health care — has published seven case studies from five countries demonstrating how data is being used to strengthen primary health care and accelerate progress towards universal health coverage (UHC). These case studies, included in the 2018 report, Measuring What Matters: Case Studies on Data Innovation for Strengthening Primary Health Care, reveal some of the ways primary health care can be supported and improved through better data collection, analysis, dissemination and use.
The countries included in this report — Argentina, Ghana, Rwanda, Senegal and Tanzania — have successfully launched innovations that strengthen how data is used to improve primary health care. As policymakers and technical experts alike gather on UHC Day 2018 to discuss ways that countries can continue to build on successes towards Health for All, the Measuring What Matters report suggests four key themes to help drive progress towards UHC:
- Local data (as well as regional and national data) should be used and shared to inform priority setting. Governments, civil society actors and donors are increasingly recognizing the importance of using local data in priority setting and the value in communicating findings and analyses back to communities. For instance, Ghana successfully scaled up its Community-Based Health Planning and Services (CHPS) program from a pilot project in three communities in one district to 4,576 communities across all of Ghana’s 216 districts by switching from a cumbersome and underutilized information management system to a new tool that was integrated with the national District Health Information Management System and enable real-time access to data on implementation and progress. Other tools simplified and streamlined data collection and made it easier to use data throughout every phase of the program’s design and implementation to pinpoint weaknesses and identify practical solutions to overcome challenges.
- Various data systems must be integrated with one another and provide a comprehensive view in order to move toward people-centered care. Promoting people-centered care means that decision-makers must be able to track patient progress across facilities and over time in order to deliver care that is responsive to the unique needs of each person. In Tanzania for example, electronic medical records are being used to share patient data across international borders, to ensure that care can be delivered continuously and in a way that fits the needs of mobile populations.
- Leveraging technology to collect, connect and disseminate data will increase coordination and continuity of care and improve access for hard-to-reach populations. Telehealth technologies and digital health solutions represent just a sample of the many ways technology is helping to redefine how health is monitored and care is delivered. In Rwanda, mobile devices enable patients to receive medical guidance at a time and place that works for them, and this is increasing accessibility in rural areas as well as coordination across providers.
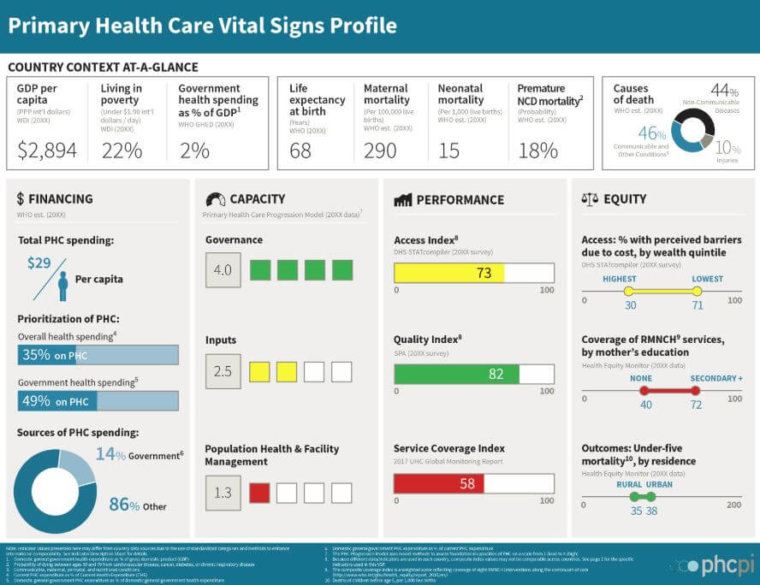
- Strengthening primary health care depends not only on the generation of new data but on the better analysis and use of existing data to identify areas of weakness and develop innovative solutions. By collecting more and better data on primary health care and using it to drive improvements, countries can take significant steps toward universal health coverage. For example, tools that use indicators to highlight areas of strength and weakness — such as PHCPI’s Vital Signs Profile — can help leaders better understand system performance and develop appropriate reforms.
As countries work to strengthen their use of data to achieve UHC, the seven case studies featured in this report show that data innovations help countries not only reach their goals but can sustain and expand improvements. Click here to learn more about how five countries are accelerating improvements in primary health care for UHC through the better use of data.